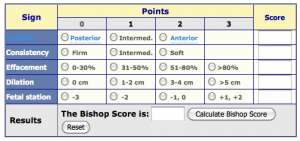
If you’re considering an elective induction or facing a medical induction, it may be helpful to know your Bishop Score. The Bishop score is a cervical assessment system, where five criteria are calculated to produce a rating between 0-13, which determines if the cervix is ready for induction. Generally, a Bishop score of 6 or below means the cervix is not ready favorable for induction.
Navigation
How is a Bishop score Calculated?
Five components are used to calculate a Bishop Score.
These components include:
- Cervical dilation – The opening of the cervix, measured in centimeters from 0-10.
- Cervical effacement – Thinness and shortening of the cervix as it stretches open, measured in percentage from 0-100%.
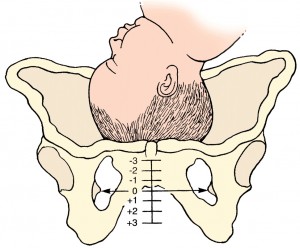
- Fetal station – The baby’s position in relation to the ischial spines of the pelvis. The ischial spines are marked “0”, above the spine is measured in “-” and below in “+”.
- Cervical consistency – Feeling of the cervix. An unfavorable cervix will feel hard, like the tip of your nose. A more favorable, soft cervix will feel like your bottom lip or the inside of your cheek.
- Cervical position – Before the onset of labor, the cervix is usually high and facing back in a posterior position behind the baby’s head. As the body gets ready for labor, the cervix will drop lower and move into a forward-facing anterior position.
BISHOP SCORE CHART
What could be the cause of a low Bishop score?
If you receive a low Bishop score, it may be because your baby is still high in the pelvis or your baby may be malpositioned in an occiput posterior position, head is asynclitic or the chin is extended. When a baby is malpositioned its head does not put adequate pressure on the cervix, which can account for a low Bishop score.
When the baby is in an optimal fetal position, the pressure of its head against the cervix leads to effacement and dilation, resulting in a higher bishop score. Rest assured, there are ways to determine and correct a malpositioned baby. (To better understand optimal fetal position, check out “Explanation of Fetal Position”).
Should I consider induction if I receive a low Bishop score?
You may consider avoiding induction if it is not medically necessary. When labor is induced before the body is ready, the odds of needing further medical intervention increase. In some situations where induction is being discussed – such as the baby being past the due date, a suspected large baby, or low amniotic fluid – you may be able to delay the induction a few days if the parent and baby are not at imminent risk. Unfortunately, many hospitals require you to schedule an induction in advance, highlighting the importance of understanding the Bishop score.
If you wish to read more information on labor induction, check out Understanding Labor Induction.
Why expectant parents should understand what a Bishop score is
At the Prenatal Yoga Center, we believe that all expectant folks should understand what a Bishop score is and at what point induction becomes necessary. This can help you to have an empowered birth and allow you to make informed decisions. We hope this information is helpful for those contemplating labor induction. Happy birthing!
Check out our series of online On Demand Classes for expectant parents for more assistance and information on birth preparation.
FAQs
How does a medical professional assess your Bishop score?
Your Bishop score is assessed by performing a manual vaginal exam where your care provider will feel your cervix. As discussed, they will check for cervical dilation, cervical effacement, cervical consistency, cervical position, and fetal positioning.
Why should I know my Bishop score?
It is useful to know your Bishop score after you have had a vaginal exam as it will tell you how close you are to labor and will help you to make an informed decision about induction.
When is a Bishop score not used?
Some conditions may mean that using a Bishop score is not helpful. For example, if you have placenta previa, a Cesarean section may be offered in which case you won’t have a vaginal exam. What’s more, if your membranes have ruptured prematurely (waters have broken), a vaginal exam might increase the risk of infection.